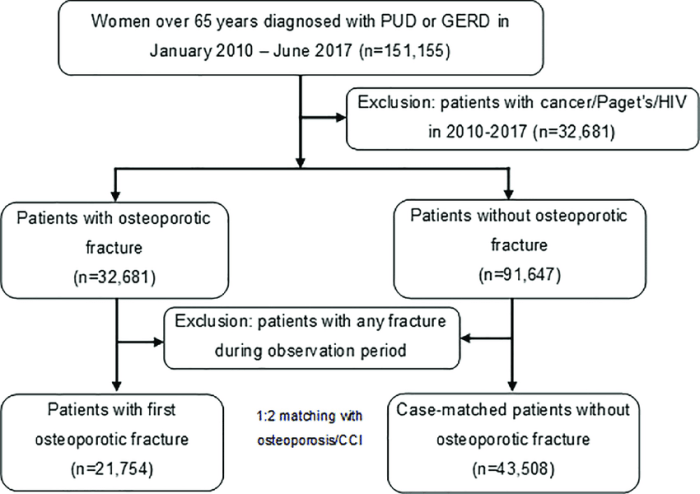
Peptic ulcer disease hesi case study takes center stage, offering a unique opportunity to delve into the intricacies of this prevalent condition. This comprehensive exploration delves into the causes, manifestations, and management of peptic ulcer disease, providing a nuanced understanding of its impact on patient health and well-being.
Through a detailed case study, we will examine the clinical presentation, diagnostic workup, and therapeutic interventions employed in the management of peptic ulcer disease in an elderly patient. This case-based approach provides a practical lens through which to appreciate the complexities of this condition and the interprofessional collaboration essential for optimal patient outcomes.
Overview of Peptic Ulcer Disease (PUD)
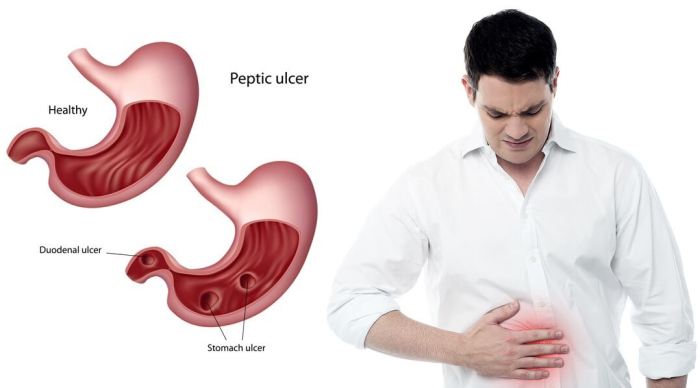
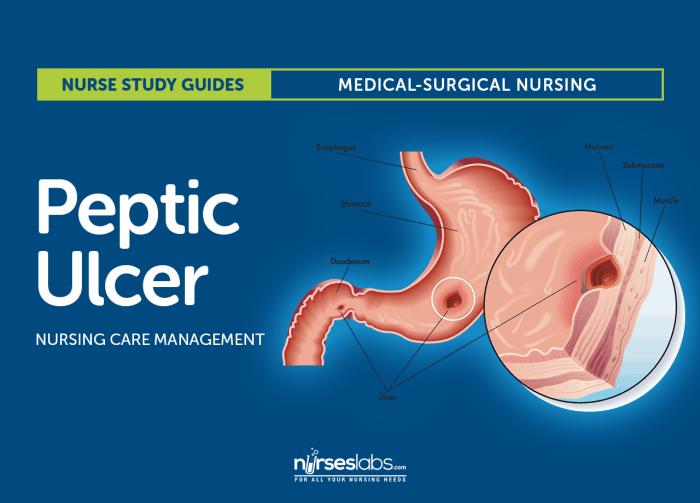
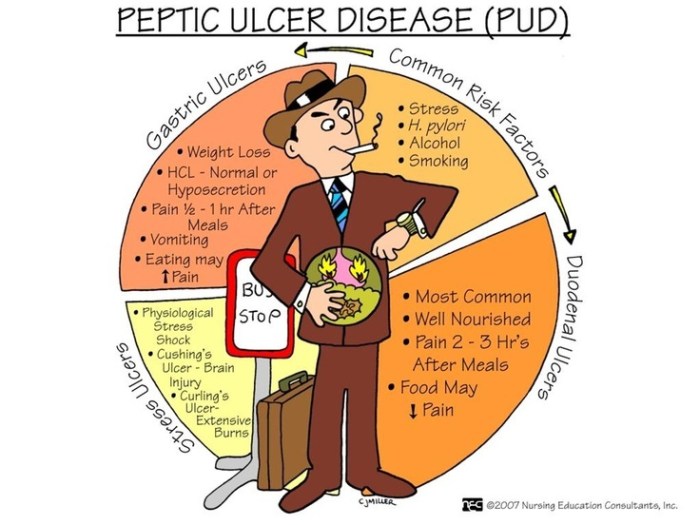
Peptic ulcer disease (PUD) is a common condition that affects the lining of the stomach and small intestine. It is caused by a break in the mucosal lining of the stomach or duodenum, allowing gastric acid and pepsin to come into contact with the underlying tissues, causing inflammation and erosion.
Causes and Risk Factors, Peptic ulcer disease hesi case study
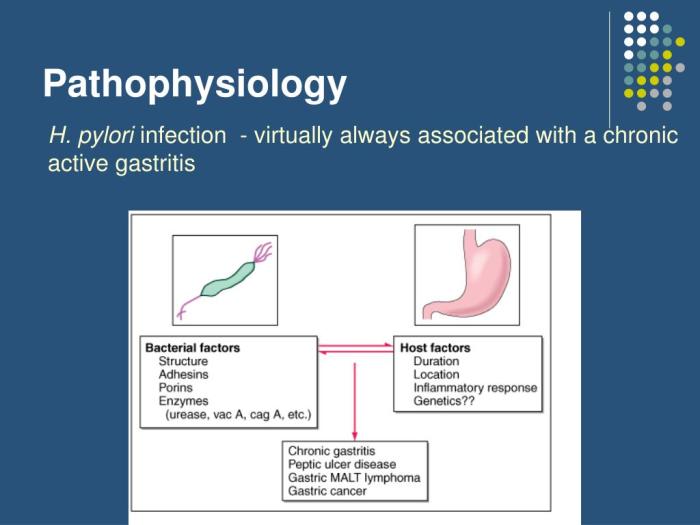
The most common cause of PUD is infection with the bacterium Helicobacter pylori( H. pylori). Other risk factors include the use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen, smoking, alcohol abuse, and stress.
Pathophysiology
PUD occurs when the protective mechanisms that normally protect the gastric mucosa from acid and pepsin are overwhelmed. This can occur due to increased acid secretion, decreased mucosal protection, or a combination of both. Acid secretion is stimulated by gastrin, a hormone produced by the stomach in response to food intake.
Mucosal protection is provided by a thick layer of mucus, bicarbonate secretion, and prostaglandin production.
Clinical Manifestations
The most common symptom of PUD is epigastric pain. The pain is typically described as a burning or gnawing sensation that occurs in the upper abdomen. Other symptoms include nausea, vomiting, bloating, and heartburn. In some cases, PUD can lead to complications such as bleeding, perforation, and obstruction.
Assessment of PUD
The assessment of peptic ulcer disease (PUD) involves a combination of patient history, physical examination, and diagnostic tests.
Patient history and physical examinationcan provide valuable information about the patient’s symptoms, duration of symptoms, and potential risk factors for PUD. The healthcare provider will inquire about the patient’s pain characteristics, including its location, severity, and timing in relation to meals. They will also ask about any associated symptoms, such as nausea, vomiting, heartburn, or indigestion.
During the physical examination, the healthcare provider will palpate the abdomen to assess for any tenderness or masses.
Diagnostic Tests
Several diagnostic tests can be used to confirm the presence of PUD and to rule out other conditions.
- Endoscopyis a procedure in which a thin, flexible tube with a camera on the end is inserted into the esophagus, stomach, and duodenum. This allows the healthcare provider to visualize the lining of these organs and to identify any ulcers or other abnormalities.
- Biopsyis a procedure in which a small sample of tissue is removed from the stomach or duodenum and examined under a microscope. This can help to confirm the diagnosis of PUD and to rule out other conditions, such as cancer.
- Stool antigen testingis a non-invasive test that can be used to detect the presence of Helicobacter pylori (H. pylori) bacteria in the stool. H. pylori is a common cause of PUD.
Treatment Options for PUD
Treatment for peptic ulcer disease (PUD) depends on the underlying cause, severity of symptoms, and individual patient factors. The primary goal of treatment is to eradicate Helicobacter pylori (H. pylori) infection, reduce gastric acid secretion, and promote ulcer healing.
Medications
Medications used to treat PUD include:
- Proton pump inhibitors (PPIs):These medications block the production of gastric acid by inhibiting the proton pump in parietal cells. Examples include omeprazole, lansoprazole, and rabeprazole.
- Histamine-2 receptor antagonists (H2RAs):These medications reduce gastric acid secretion by blocking histamine-2 receptors on parietal cells. Examples include ranitidine, famotidine, and cimetidine.
- Antacids:These medications neutralize gastric acid and provide temporary relief from symptoms. Examples include calcium carbonate, magnesium hydroxide, and aluminum hydroxide.
- Antibiotics:Antibiotics are used to eradicate H. pylori infection. The standard regimen includes a combination of amoxicillin, clarithromycin, and a PPI.
The efficacy and side effects of common PUD medications are summarized in the following table:
| Medication | Efficacy | Side Effects |
|---|---|---|
| PPIs | High | Headache, diarrhea, nausea, abdominal pain |
| H2RAs | Moderate | Headache, diarrhea, nausea, abdominal pain |
| Antacids | Low | Constipation, diarrhea, nausea, abdominal pain |
| Antibiotics | High | Diarrhea, nausea, vomiting, abdominal pain |
Lifestyle Modifications
Lifestyle modifications can help reduce symptoms and prevent recurrence of PUD, including:
- Avoiding smoking
- Limiting alcohol consumption
- Eating a healthy diet low in spicy, fatty, or acidic foods
- Maintaining a healthy weight
- Managing stress
Surgery
Surgery may be necessary in cases of severe or refractory PUD. Surgical options include:
- Vagotomy:This procedure involves cutting the vagus nerve, which stimulates gastric acid secretion.
- Antrectomy:This procedure involves removing the antrum of the stomach, which is the site of most acid production.
- Gastrectomy:This procedure involves removing all or part of the stomach.
Nursing Management of PUD
Nurses play a pivotal role in the management of PUD by providing patient education, support, and implementing interventions to alleviate symptoms and prevent complications.
Patient education involves informing individuals about the causes, risk factors, and lifestyle modifications that can help prevent and manage PUD. Nurses educate patients on the importance of avoiding tobacco, alcohol, and NSAIDs, as well as adopting a healthy diet and stress management techniques.
Nursing Interventions for Symptom Management and Prevention of Complications
Nurses implement various interventions to manage symptoms and prevent complications of PUD. These include:
- Pain Management:Nurses administer pain medications, such as proton pump inhibitors (PPIs) or histamine-2 receptor antagonists (H2RAs), to reduce gastric acid production and relieve pain.
- Diet Modification:Nurses collaborate with dieticians to develop personalized dietary plans that minimize gastric irritation and promote healing. This may include avoiding spicy, acidic, or fatty foods, and eating smaller, more frequent meals.
- Stress Reduction:Nurses provide stress management techniques, such as deep breathing exercises or meditation, to help patients cope with stress, which can exacerbate PUD symptoms.
- Smoking Cessation Support:Nurses assist patients in quitting smoking by providing resources and support, as smoking is a major risk factor for PUD.
- Monitoring for Complications:Nurses closely monitor patients for signs and symptoms of complications, such as bleeding, perforation, or obstruction, and promptly report any concerns to the healthcare team.
Case Study
Introduction:Peptic ulcer disease (PUD) is a common condition that affects the lining of the stomach and small intestine. It is more common in elderly patients due to age-related changes in the gastrointestinal tract, including decreased gastric acid secretion, impaired mucosal defense mechanisms, and increased use of nonsteroidal anti-inflammatory drugs (NSAIDs).
This case study presents an elderly patient with PUD and discusses the patient’s history, physical examination findings, diagnostic tests, and treatment plan.
Patient History
The patient is a 75-year-old male who presents with a 2-week history of epigastric pain, nausea, and vomiting. He has a history of hypertension, hyperlipidemia, and gastroesophageal reflux disease (GERD). He takes aspirin daily for his cardiovascular disease and omeprazole for his GERD.
He denies any recent trauma or surgery.
Physical Examination Findings
On physical examination, the patient is afebrile and has normal vital signs. His abdomen is soft and non-tender, with no palpable masses or organomegaly. Bowel sounds are present in all four quadrants.
Diagnostic Tests
An upper endoscopy is performed, which reveals a 2-cm ulcer in the gastric antrum. The ulcer is shallow and non-bleeding. A biopsy of the ulcer is taken, which shows no evidence of malignancy.
Treatment Plan
The patient is started on a proton pump inhibitor (PPI), such as omeprazole or lansoprazole, to reduce gastric acid secretion and promote ulcer healing. He is also advised to avoid NSAIDs and alcohol, which can irritate the stomach lining. The patient is followed up closely with repeat endoscopies to monitor ulcer healing and ensure complete resolution.
Interprofessional Collaboration in PUD Management
Interprofessional collaboration is crucial in managing PUD effectively, as it involves a multifaceted approach that requires expertise from various healthcare professionals. This collaborative approach ensures comprehensive patient care, addressing the medical, psychological, and lifestyle factors contributing to PUD.
Roles of Healthcare Professionals in PUD Care
- Physicians:Diagnose PUD, prescribe medications (e.g., PPIs, antibiotics), and perform endoscopic procedures (e.g., upper endoscopy).
- Nurses:Educate patients about PUD, monitor symptoms, administer medications, and provide lifestyle counseling.
- Pharmacists:Ensure appropriate medication use, monitor for drug interactions, and provide patient education.
- Dietitians:Provide nutritional guidance, recommend dietary modifications, and help patients manage their weight.
- Psychologists:Address stress-related factors that may contribute to PUD, provide coping mechanisms, and offer support.
Evidence-Based Practice in PUD Management: Peptic Ulcer Disease Hesi Case Study
Evidence-based practice (EBP) is a systematic approach to clinical decision-making that incorporates the best available research evidence, clinical expertise, and patient values. In PUD management, EBP involves using current guidelines and research findings to guide diagnosis, treatment, and patient education.
Current Evidence-Based Guidelines
The American College of Gastroenterology (ACG) and the European Society of Gastrointestinal Endoscopy (ESGE) have developed evidence-based guidelines for the diagnosis and management of PUD. These guidelines recommend:
- Upper endoscopy as the gold standard for diagnosing PUD.
- Proton pump inhibitors (PPIs) as the first-line treatment for uncomplicated PUD.
- Helicobacter pylori (H. pylori) eradication therapy for H. pylori-positive PUD.
- Endoscopic therapy for bleeding or perforated ulcers.
Latest Research Findings
Recent research has further refined the management of PUD. Some key findings include:
- PPIs are more effective than histamine-2 receptor antagonists (H2RAs) in healing PUD.
- Triple therapy (PPI, amoxicillin, and clarithromycin) is more effective than dual therapy (PPI and amoxicillin) for H. pylori eradication.
- Endoscopic therapy is safe and effective for bleeding or perforated ulcers.
Query Resolution
What are the common symptoms of peptic ulcer disease?
Abdominal pain, heartburn, nausea, vomiting, and weight loss are common symptoms of peptic ulcer disease.
What are the risk factors for developing peptic ulcer disease?
Helicobacter pylori infection, use of nonsteroidal anti-inflammatory drugs (NSAIDs), smoking, and excessive alcohol consumption are major risk factors for peptic ulcer disease.
How is peptic ulcer disease diagnosed?
Peptic ulcer disease is typically diagnosed through endoscopy, which involves inserting a thin, flexible tube with a camera into the esophagus, stomach, and duodenum to visualize the lining of these organs.